Retina: The window to your vision.
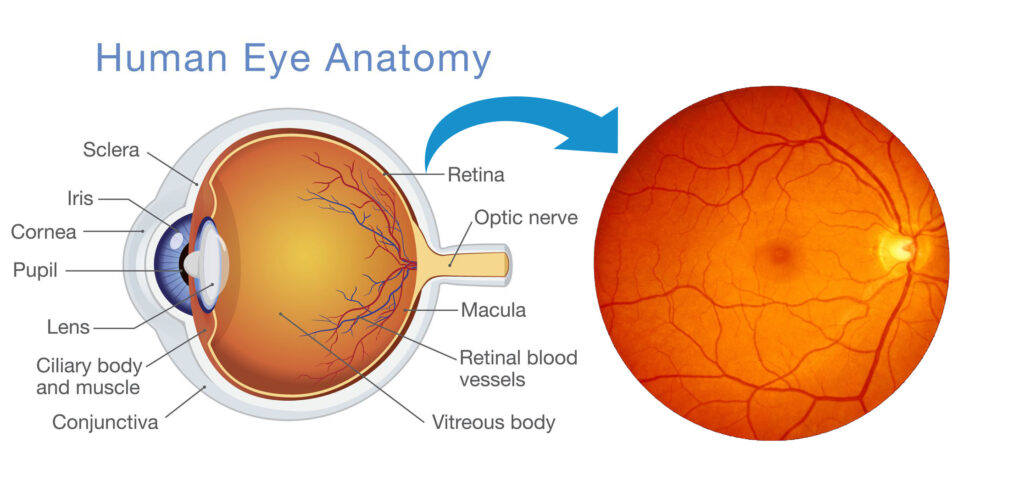
The retina is a light-sensitive layer of tissue lining the back of the eyeball. It’s responsible for converting light that enters the eye into electrical signals that are transmitted to the brain, allowing us to see. Imagine the retina as the film in a camera, capturing light and translating it into an image.
- Function: When light enters the eye, it passes through the cornea, pupil, lens, and vitreous humor before reaching the retina. The photoreceptor cells in the retina, called rods and cones, absorb light and convert it into electrical signals. These signals are then processed by other cells in the retina before being sent to the brain via the optic nerve.
- Importance: The retina is essential for vision. Damage to the retina can lead to vision loss, so it’s important to maintain good eye health and have regular eye exams.
Retinal Conditions
Early detection and treatment of retinal conditions can help prevent vision loss. If you experience any sudden changes in your vision, such as blurred vision, floaters, or flashes of light, see an eye doctor right away.
What is Retinal Detachment?
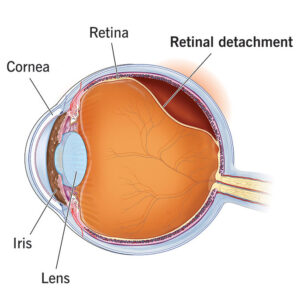
Retinal detachment is a disorder of the eye in which the retina peels away from its underlying layer of support tissue. Initial detachment may be localized, but without rapid treatment the entire retina may detach, leading to vision loss and blindness. It is a surgical emergency.
Symptoms
Retinal detachment itself is painless. But warning signs almost always appear before it occurs or has advanced, such as:
- The sudden appearance of many floaters — tiny specks that seem to drift through your field of vision
- Flashes of light in one or both eyes (photopsia)
- Blurred vision
- Gradually reduced side (peripheral) vision
- A curtain-like shadow over your field of vision
What is Diabetic Retinopathy?
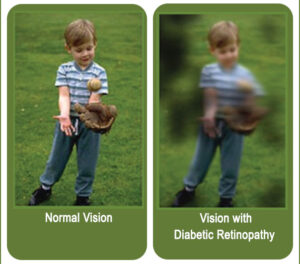
Diabetic retinopathy, is a medical condition in which damage occurs to the retina due to diabetes. It is a leading cause of blindness in developed countries. Diabetic retinopathy affects up to 80 percent of those who have had both type 1 and type 2 diabetes for 20 years or more.
Symptoms
You might not have symptoms in the early stages of diabetic retinopathy. As the condition progresses, you might develop:
- Spots or dark strings floating in your vision (floaters)
- Blurred vision
- Fluctuating vision
- Dark or empty areas in your vision
- Vision loss
When to see an eye doctor
Careful management of your diabetes is the best way to prevent vision loss. If you have diabetes, see your eye doctor for a yearly eye exam with dilation — even if your vision seems fine.
Developing diabetes when pregnant (gestational diabetes) or having diabetes before becoming pregnant can increase your risk of diabetic retinopathy. If you’re pregnant, your eye doctor might recommend additional eye exams throughout your pregnancy.
Contact your eye doctor right away if your vision changes suddenly or becomes blurry, spotty or hazy.
What is Macular Degeneration?
Macular degeneration, also known as age-related macular degeneration (AMD), is a medical condition which may result in blurred or no vision in the center of the visual field. Early on there are often no symptoms. Over time, however, some people experience a gradual worsening of vision that may affect one or both eyes.
AMD affects the central vision, and with it, the ability to see fine details. In AMD, a part of the retina called the macula is damaged. In advanced stages, people lose their ability to drive, to see faces, and to read smaller print. In its early stages, AMD may have no signs or symptoms, so people may not suspect they have it.
Types of Age-Related Macular Degeneration and Causes
The two primary types of age-related macular degeneration have different causes:
Dry. This type is the most common. About 80% of those with AMD have the dry form. Its exact cause is unknown, although both genetic and environmental factors are thought to play a role. This happens as the light-sensitive cells in the macula slowly break down, generally one eye at a time. The loss of vision in this condition is usually slow and gradual. It is believed that the age-related damage of an important support membrane under the retina contributes to dry age-related macular degeneration.
Wet. Though this type is less common, it usually leads to more severe vision loss in patients than dry AMD. It is the most common cause of severe loss of vision. Wet AMD happens when abnormal blood vessels start to grow beneath the retina. They leak fluid and blood — hence the name wet AMD — and can create a large blind spot in the center of the visual field.
Risk Factors for Age-Related Macular Degeneration
There are several risk factors that can contribute to developing age-related macular degeneration, including:
Being 50 and older
Eating a diet high in saturated fat
Smoking
High blood pressure or hypertension
Symptoms
The following are the most common symptoms of AMD. However, each individual may experience symptoms differently. Symptoms may include:
Blurry or fuzzy vision
Difficulty recognizing familiar faces
Straight lines appear wavy
A dark, empty area or blind spot appears in the center of vision
Loss of central vision, which is necessary for driving, reading, recognizing faces and performing close-up work
The presence of drusen, which are tiny yellow deposits in the retina, is one of the most common early signs of age-related macular degeneration. It may mean the eye is at risk for developing more severe age-related macular degeneration. These will be visible to your doctor during an eye exam.
The symptoms of age-related macular degeneration may look like other eye conditions. Speak with an eye care professional for diagnosis.

What is Diplopia?
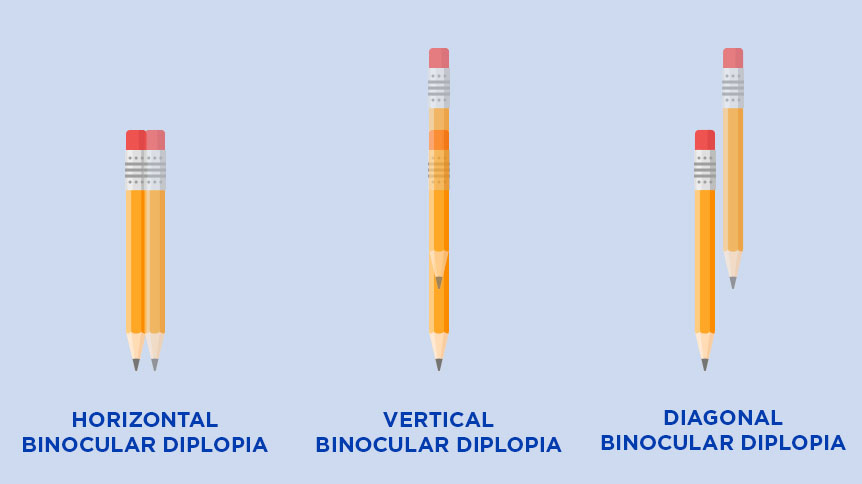
Diplopia is the simultaneous perception of two images of a single object that may be displaced horizontally or vertically in relation to each other. Also called double vision, it is a loss of visual focus under regular conditions, and is often voluntary. Two main types of double vision exist:
Monocular diplopia occurs when someone sees double vision with only one eye open, a second image usually appearing as “a ghost.” Causes are typically confined to the eye and less likely to be neurological.
Binocular diplopia occurs when someone sees double vision only when both eyes are open. Causes may be serious conditions, neurological or otherwise.
Symptoms
Other than seeing double, diplopia can be associated with other symptoms like:
- Headache.
- Nausea (upset stomach or feeling sick).
- Dizziness.
- Pain (including when you move your eyes).
- Blurred or unclear vision in one or both eyes.
Management and Treatment
Double vision is treated depends on what’s causing it. Talk to your healthcare provider about the cause of your diplopia and what needs to be done to correct it.
What are Floaters?
Floaters or eye floaters are sometimes visible deposits within the eye’s vitreous humour, which is normally transparent, or between the vitreous and retina. They can become particularly noticeable when looking at a blank surface or an open monochromatic space, such as blue sky.
Symptoms
Symptoms of eye floaters may include:
- Small shapes in your vision that appear as dark specks or knobby, transparent strings of floating material
- Spots that move when you move your eyes, so when you try to look at them, they move quickly out of your line of vision
- Spots that are most noticeable when you look at a plain bright background, such as a blue sky or a white wall
- Small shapes or strings that eventually settle down and drift out of the line of vision
When to see a doctor
Contact an eye specialist immediately if you notice:
- Many more eye floaters than usual
- A sudden onset of new floaters
- Flashes of light in the same eye as the floaters
- A gray curtain or blurry area that blocks part of your vision
- Darkness on a side or sides of your vision (peripheral vision loss)
These painless symptoms could be caused by a retinal tear, with or without a retinal detachment. This is a sight-threatening condition that requires immediate attention.

What is Photopsia?
Photopsia is the presence of perceived flashes of light in the field of vision.
Vitreous shrinkage or liquefaction, which are the most common causes of photopsia, cause a pull in vitreoretinal attachments, irritating the retina and causing it to discharge electrical impulses. These impulses are interpreted by the brain as flashes.
Photopsia can present as retinal detachment when examined by an ophthalmologist. Photopsia should be investigated immediately.
What do photopsias (eye flashes) look like?
The flashes of light you may see in your eyes are most likely to be white or sparkly, but colored lights happen, too. The flashes can take many shapes, including:
- Zigzag lines.
- Streaks of lightning.
- Brief pops like flashbulbs going off.
- Sparks or flickering lights.
- Flashes that spin in circles.
- Spots or thick lines.
- White snow or fuzz.

This is an approximation of the zig-zag visual disturbance that I experience as a migraine aura. The picture hardly does it justice! In reality it moves and vibrates, expanding and slowly fading away over the course of about 20 minutes.
Usefull Links
Information
Monday to Saturday
Morning: 11:00 am to 2:00 pm
Evening 7:00 pm- 9:00 pm
Sunday Closed

